Radiology Positioning Guide – This chapter is designed as a quick reference for radiographic placement and technique. Technical advice and additional insights are provided to help achieve optimal film quality using the most appropriate approaches. Normal examination is highlighted in blue; that is, for a complete assessment of the area in question, minimum views to be made. For more information on the approaches covered in this chapter, the textbook dedicated to radiographic positioning should be consulted. A list of recommended further reading is included at the end of this section.
The basic components of a radiography unit are a radiation source (X-ray tube) and a receiving medium (X-ray film in conventional plain film radiography or energized plate in computed radiography). Figures 3-1 and 3-2 identify the stool, table, shields, side markers, and other accessories used in the radiographic setup.
Radiology Positioning Guide

FIGURE 3-1 Typical radiographic system and related equipment, including: A, network cabinet (Bucky); B, X-ray tube; C, collimator; D, mobile table; E, positioning sponge; and F, feces.
Emrad: Radiologic Approach To The Traumatic Shoulder
FIGURE 3-2 Instruments and accessories used in radiographic examinations, including A, measuring instruments; B, lead apron; C, latent female gonad; D, latent male gonad; E, right and left (Mitchell) marks; F, filters; G, cassettes; and H, to locate the sponges.
The proposed technique is within a fixed kilovolt (kV) range for each body part. In smaller patients, the low V range is used; in larger patients the upper kV range is used. In this system, milliampere-seconds (mAs) are variable, and exposure factor correction requires changing only the mAs. To correct the exposure factors on an underexposed film, the mAs must be changed by at least 30% for a detectable change or 100% for a significant change. The opposite is true for overexposed films. When using a fixed KV system, only one exposure factor, mAs, must be changed to correct errors. The techniques listed in the table provide a starting point for appropriate exposures for a radiographic system similar to the one listed. Corrections for individual machine variations are made by adjusting mAs only because the table is formulated using fixed kV technique.
There may be cases where a change in penetration, or kVp, is required. When critiquing a film whose skeletal details are too distinct to exist, a 15% increase in kVp provides the necessary penetration. An increase in mAs is needed if there is bone detail, but the overall look of the film is too light.
Good patient education is essential and should include a thorough explanation of the examination being carried out and the patient’s role during the examination. Protective methods and breathing instructions should be reviewed. Patients should be properly dressed, and all artifacts should be removed before the radiographic examination begins (Figure 3-3). Pregnant female patients should be assessed for possible pregnancy. If there is a possibility of pregnancy, the examination should be postponed if possible until it is established that the patient is not pregnant, either by a negative test result for human chorionic gonadotropin or by the onset of menstruation. If possible, all X-rays of the lower back, abdomen and pelvis should be scheduled within the first 10 days after the start of menstruation, which is the shortest time before pregnancy occurs. Appropriate gonadal protection should be used whenever possible in both male and female patients.
Radiographic Positioning Examples Of The Leg And Knee
3-3 IMAGE X-ray setup is most skillful following a general sequence. The sequence begins with patient preparation, including A, one; then B, choice of measurement technique; C, cassette selection and placement; D, select focal film distance; E, location of central rays; F, film center and center beam adjustment. G, film size collimation; H, location of lateral markings; and sometimes I use the filter.
The following tables show the commonly performed X-ray projections. Normal examination is highlighted in blue. A normal survey is the minimum number of views required to obtain a complete survey of the field. Additional views are included in most sections and can be added to the core study. Additional views are added to better display a current area or to assess movement or stability. For reference, radiographs are designated by the body part being examined and the direction that the radiographic beam passes through the body (anteroposterior [AP]) or by the part of the body portal touching the grid for oblique angles of the body (right). posterior oblique [RPO]) (3 Figure -4).
FIGURE 3-4 Radiographs. The radiographic term “projection” refers to the path of the central beam exiting the X-ray tube and passing through the patient’s body. For example, A represents the anteroposterior (AP) projection and B represents the anteroposterior (PA) projection. At the ends the lateral projections are similarly described by the direction of the central ray; therefore, medial and lateral-medial projections are possible. However, when the head, neck, or trunk is involved, the lateral and oblique protrusions become even more apparent depending on the exact “position” of the patient. Position represents the location of the patient’s body, specifically the part of the patient’s anatomy that is in contact with Bucky. For example, C represents side projection in the right side position, and D represents side projection in the left side position. In E, the patient is in left anterior oblique position (LAO), and in F, the patient is in right anterior oblique position (RAO), both corresponding to PA oblique projections.

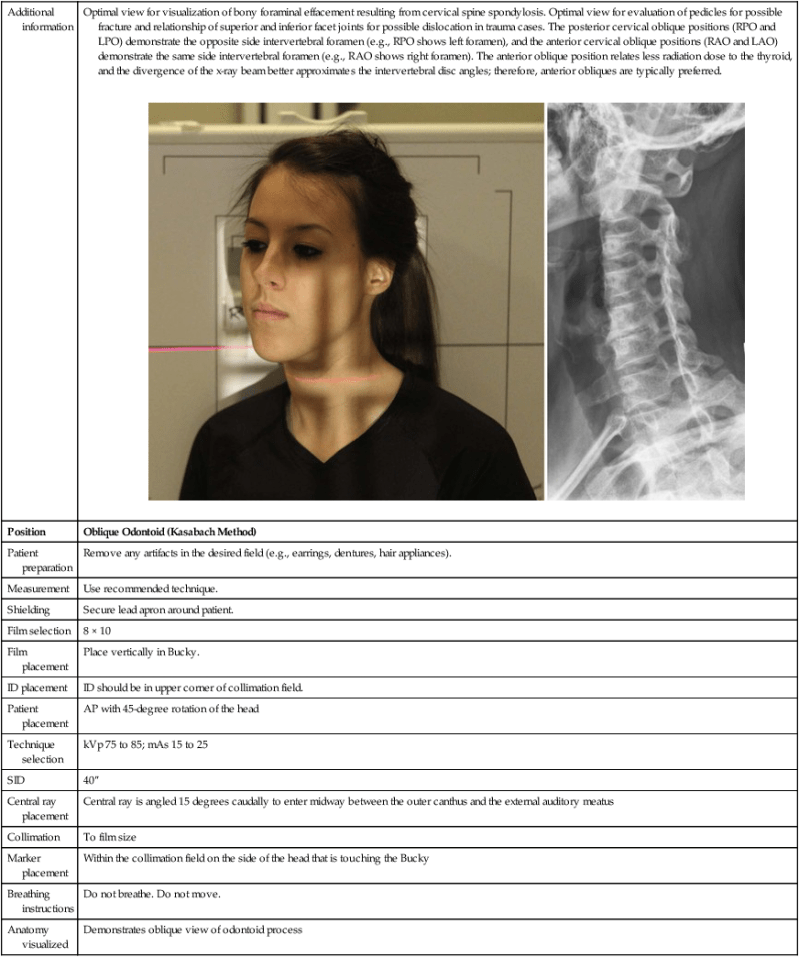
Each diagram describes the position setup, center beam placement, tube angulation, optimal film size, and focal film distance for each view. To preserve the X-ray film and make it easier to view, the film is sometimes split so that multiple views of a body part can be seen on a single film (Figure 3-5). For each configuration in the tables, there is one image showing the position and location of the central rays and another to show the anatomy shown by the configuration. The kV and mAs section shows what type of film screen combination is used and whether the examination is performed using a grid or table. If the use of a grid is listed, a fast film screen combination such as rare earths is suggested. If detail or gridless is listed, a combination of slower film screens, such as those found on extreme cassettes or 100-speed cassettes, is suggested. The kV and mAs range is suggested for the systems described in the previous section on technique. The “Additional Information” section describes other views that can be performed to better demonstrate the desired anatomy. Technical tips are also included to help you achieve optimal learning.
Positioning Tips For Dental Radiographs — New Vet Equipment
FIGURE 3-5 A to D. For some small body parts (such as the foot and wrist), the x-ray film may be split to accommodate more protrusions. From Ballinger PW, Frank ED: Merril’s atlas of radiographic positions and radiologic procedures, 10th ed., St. Louis, 2003, Mosby.
Place the base of the caliper on the back of the skull. Slide the caliper arm until it rests lightly against the nation.
Using a caudal tube slope of 15 degrees, the central rays enter the back of the skull to exit the nation.
Frontal bone, frontal and ethmoid sinuses, greater and lesser wing of sphenoid, superior orbital fissure, foramen around, orbital rims
Radiographic Positioning And Related Anatomy Apk For Android Download
The angle of the caudal tube can be increased to 30 degrees to properly define the lower orbital rim area. The oil pyramids appear in the lower third of the path as in the previous view. These project below the lower orbital rim at an angle of 30 degrees.
Place the caliper base rod on the rear head. Push the movable rod towards the patient’s head to touch the glabella.
Place the patient in the AP position with the back of the head touching the Bucky. Position the chin so that the orbitomeatal line is perpendicular to the film.

If the patient cannot insert the chin correctly, adjust the head tilt so that the infraorbitomeatal line is perpendicular to the film and increase the tube tilt to ≈37 degrees.
Free Radiology Apps
Place the base rod of the calipers on the temporal bone on one side of the head and move the slider toward the patient’s head to touch the temporal bone on the other side of the head.
Position the patient with the side of the head facing the Bucky. Patient’s body for comfort. The interpupillary line is perpendicular to the film. The external occipital protuberance and nasion must be equidistant from the film to prevent rotation.
Place the base bar of the calipers on the back of the skull and move the caliper toward the patient’s face until it touches between the lower lip and the tip of the chin.
The center beam is directed perpendicular to Bucky and is centered on the center of the cassette.
Bontrager’s Textbook Of Radiographic Positioning Test Bank
It should be performed in an upright position to assess the air-fluid level in the maxillary sinuses. The petrosal ridges should protrude into the lower half of the maxillary sinus below the lower orbital rim. A good approach to assess path disturbances for possible “bursts”.
Position the base rod to the calipers
Radiology positioning and techniques, positioning in radiology, radiology positioning, radiology positioning book, radiology positioning quiz, radiology positioning aids, radiology positioning pocket guide, positioning sponges for radiology, radiology positioning sponges, veterinary radiology positioning guide, radiology positioning devices, veterinary radiology positioning